

The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber.
The cornea can be reshaped by surgical procedures such as LASIK
The human cornea has five layers
1. Corneal epithelium: fast-growing and easily regenerated cells, kept moist with tears. Irregularity or edema of the corneal epithelium disrupts the smoothness of the air/tear-film interface, the most significant component of the total refractive power of the eye, thereby reducing visual acuity.
2. Bowman's layer (also known as the anterior limiting membrane)

3. Corneal stroma: Corneal stroma (also substantia propria): a thick, transparent middle layer, consisting of regularly arranged collagen fibers.
4. Descemet's membrane (also posterior limiting membrane): a thin acellular layer
5. Corneal endothelium: a simple squamous or low cuboidal monolayer, of mitochondria-rich cells. These cells are responsible for regulating fluid and solute transport between the aqueous and corneal stromal compartments. The corneal endothelium is bathed by aqueous humor. Unlike the corneal epithelium, the cells of the endothelium do not regenerate. Instead, they stretch to compensate for dead cells which reduces the overall cell density of the endothelium, which affects fluid regulation. If the endothelium can no longer maintain a proper fluid balance, stromal swelling due to excess fluids and subsequent loss of transparency will occur and this may cause corneal edema and interference with the transparency of the cornea.
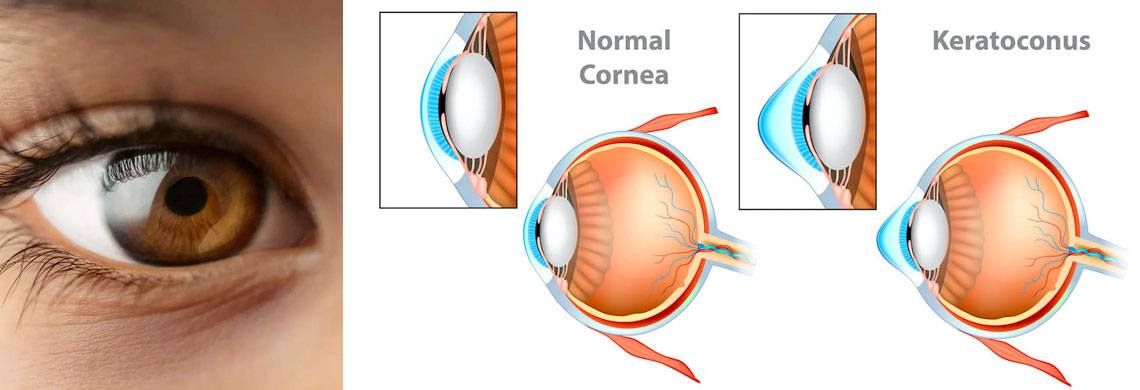
Keratoconus (from Greek: kerato- horn, cornea; and konos cone) is a degenerative disorder of the eye in which structural changes within the cornea cause it to thin and change to a more conical shape than its normal gradual curve. Grossly the eye is more ‘cone’ shaped rather than the usual football or rugby ball shape.
Keratoconus can cause substantial distortion of vision, with multiple images, streaking and sensitivity to light. If afflicting both eyes, the deterioration in vision can affect the patient’s ability to drive a car or read normal print.
It is typically diagnosed in the adolescent years and attains its most severe state by the age of 30 (although this is variable).
Keratoconus affects around one person in a thousand. It seems to occur in populations throughout the world, although it is observed more frequently in certain ethnic groups, such as Asians. Environmental and genetic factors are considered possible causes, but the exact cause is uncertain. It is more common in patients with asthma, eczema and hayfever.

Some cases of keratoconus are mild and only result in the need for glasses. However, in most eyes the condition progresses and the cornea bows forward in an irregular manner. This irregular bowing of the cornea means that glasses or normal soft contact lenses are unable to give clear vision and such individuals may then require hard contact lenses in order to see. These hard lenses help the majority with keratoconus.
Other options include corneal ring segment inserts (Intacs or Ferrara rings), or topography-guided laser only to remove slight irregularity (not to remove prescription) and phakic implants. These are for people with stable keratoconus.
However, keratoconus typically progresses up to the age of 30 necessitating changes in contact lenses and ultimately it is possible that contact lenses are no longer effective in restoring sight.
The only option is then to consider corneal transplantation (replacing the central cornea with donated corneal tissue). This is a major surgical procedure on the eye needing life long review with a risk of 1 in 500 of blindness and hence avoided if at all possible.
There are risks transplant rejection, unpredictable visual outcomes, and development of high astigmatism. The advantages of postponing a transplant are many; even following a successful procedure, the mean survival rate of a penetrating transplant is about 17 years (many have to repeat the procedure).



Yes. Cross-linking (also known as CXL, CCR, CCL and KXL) is a surgical treatment for keratoconus.
Corneal collagen cross-linking is a process whereby bonds form between collagen molecules within the structure of the cornea to stiffen its structure. Collagen is the main structural protein of the cornea. Corneal collagen cross-linkage occurs naturally with age and this process can be accelerated using a combination of riboflavin (vitamin B) eye drops and ultraviolet light shone at the cornea. It has been shown to strengthen the cornea. In keratoconus, it appears to prevent progression and may occasionally reverse the corneal bowing to a certain extent.
Cross linking was first developed in Germany in 2000 and clinical trials started the same year. In Italy, this has also been successfully performed since 2002. The procedure has been in routine use in Europe for a number of years with trials showing greater than 95% success rate. Results from an Australian study published in 2008 showed stabilisation in all treated eyes, and a slight correction in visual acuity in most patients.
The aim is to stabilise the cornea and prevent progression of the keratoconus. In a small portion of people, there is a slight improvement in the shape of the cornea and hence the vision but this is not guaranteed.
The 2 types of cross linking are epithelium on or epithelium off. we prefer epithelium off as we have had excellent results with this and do not want to take the chance of the treatment not working because the epithelium is on.
Anaesthetic drops are applied to the eye.
The epithelium (the top layer of the cornea) is loosened and removed in the centre.
A sticky yellow fluid, Riboflavin, is put on to this area for 20-30 minutes.
The treatment is commenced for 30 minutes in 6 five minute steps. The patient needs to concentrate on a flashing light in the centre of the instrument.
It is useful to bring an iPod in as otherwise this is a long and boring procedure.
The recovery is 3-5 days from the surgery. A stable situation is reached by 4-6 weeks.
A slight, superficial haziness of the cornea has been seen in some patient in the first few weeks after treatment. This is transient and disappears by 6-8 weeks. It does not permanently impair vision.
Following treatment, it is possible to experience 24 to 72 hours of eye discomfort while the skin over-lying the corneal heals (the epithelium). Painkillers will be prescribed to alleviate this pain.
There is a risk of infection as with any operation. To prevent this potential complication, the procedure will be conducted under sterile conditions and antibiotics eye drops will be prescribed after the treatment.
For visual rehabilitation, spectacles are useful in mild keratoconus. However, due to compromised visual quality and sub-optimal vision, most patients are unsatisfactory with the spectacles.
Contact lenses provide the advantage of masking the irregular corneal surface and thereby providing dramatic improvement in the visual acuity in most cases.At Manav Hospital we are equipped with contact lens specialist for this treatment.
Rigid gas permeable (RGP) lenses, hybrid lenses, Rose-K lenses, mini-scleral and scleral lenses are some of the commonly used lenses in keratoconus.
INTACS, Corneal Inserts or Intracorneal Ring Segments: In patients who are contact lens intolerable or in patients who does not want to wear contact lens but need better visual quality with spectacles, intrastromal corneal ring segments (INTACS), which look like half-moon shaped clear plastic rings, could be useful.
Single or double INTACS rings could be placed in the mid-peripheral cornea depending on the patient’s topographic and refractive parameters.
This procedure does not prevent progression; however, this could help to regularize corneal surface and centre the cone thereby improving the corrected visual quality or contact lens tolerance.
This procedure could be combined with CXL to prevent progression.
It could be used in the management of keratoconus to modify the corneal anatomy using excimer laser. At Manav Hospital we are equipped with the best Laser Ex 500 for this treatment.
This procedure attempts to improve the central corneal symmetry rather than correction of the patient’s refractive errors, thereby altering minimal corneal tissue of up to 50 microns. This procedure is done after removal of the corneal epithelium using phototherapeutic keratectomy (PTK). Hence, T-CAT could result in improvement of the corneal topography and corrected distance visual acuity.
This procedure could also be combined with various CXL protocols.
ICLs are micro thin lenses implanted over the natural lens, inside the eye, to correct spectacle power.
They are similar to contact lenses placed in eyes except that a contact lens is temporary and has to be put on a daily basis whereas ICL is put inside the eye permanently.
It is a viable option for visual rehabilitation if the Keratoconus patient requires independence from spectacle or contact lenses.
Eyes having CXL or C3R tend to have a fluctuation in refraction in the initial post-treatment. After the refraction stabilizes (may take up to 3 months), these patients may be offered ICL surgery.
Toric ICLs are especially useful in patients with astigmatism.
In cases of patients with severe scarring in the visual axis or advanced keratoconus with progressive thinning with unstable contact lens fit and poor visual acuity, eye doctors prefer to replace the cornea with a donated cornea, the surgery is called Keratoplasty.
Depending on the extent of scarring and corneal thickness, your surgeon may decide to perform a full thickness procedure called Penetrating Keratoplasty (PK), or a partial thickness procedure called Deep Anterior Lamellar Keratoplasty (DALK).
